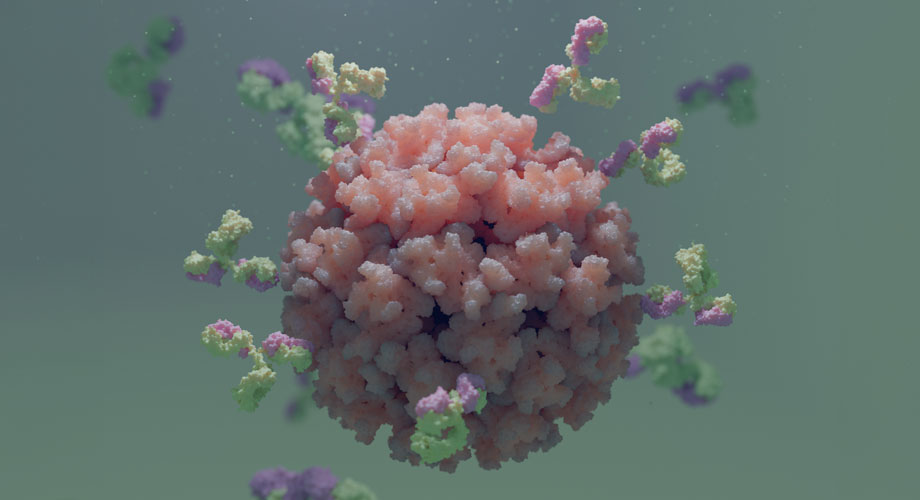
Caption: Antibodies binding to Venezuelan Equine Encephalitis virus (VEEV). Credit: Scripps Research
Scripps Research scientists receive up to $12M to create universal vaccine for alphaviruses
Funding from ARPA-H will be used to develop a vaccine for alphaviruses in preparation of major outbreaks in the U.S.
December 04, 2024
LA JOLLA, CA—Alphaviruses often cause a range of illnesses that lead to fever, rash and debilitating joint pain. While they’re historically prevalent in tropical and subtropical regions of the world where virus-transmitting mosquitos are abundant, these mosquitos are expanding to new terrain—including the U.S.—as global warming intensifies. Alphavirus diseases like eastern equine encephalitis, which inflames the brain and can lead to death, are among the country’s emerging threats against which no human vaccine is available.
Despite various efforts in the works to develop vaccines for specific alphaviruses, there’s currently no “universal” vaccine to broadly target a range of virus strains. That means as alphaviruses become more widespread, people will need several jabs rather than one—assuming specific vaccines become available.
Now, a collaboration among Scripps Research, Vanderbilt University and others has been awarded more than $46 million from the Advanced Research Projects Agency for Health (ARPA-H), a research funding agency of the U.S. government, to develop a universal vaccine against alphaviruses. Scripps Research will receive up to $12 million for its contribution to the project, which is expected to last five years.
The principal investigators at Scripps Research include Torben Schiffner, PhD, who leads immunogen design at the institute; Darrell Irvine, PhD, a professor in the Department of Immunology and Microbiology; Andrew Ward, PhD, a professor in the Department of Integrative Structural and Computational Biology; and Ian Wilson, PhD, who chairs the Department of Integrative Structural and Computational Biology and is the Hansen Professor of Structural Biology.
“This award combines experts in artificial intelligence (AI) with vaccinologists to accomplish a great deal over a short time span,” says Schiffner, who is the lead principal investigator on the award at Scripps Research. “We’re going to hear a lot more about alphaviruses in the future, and there already have been minor outbreaks in the U.S.”
The money from ARPA-H will fund a two-stage project: After a three-year preclinical stage to create an immunogen candidate, the molecule will enter a phase 1 clinical trial for two years if it performs well preclinically. An immunogen is a substance that activates the immune system, helping the body recognize and fight harmful agents like viruses. This is a primary step in vaccine development, as scientists design an immunogen to mimic parts of a virus—that way, when the resulting vaccine is administered, the body can learn how to defend itself even if it has never been exposed to the actual virus.
The principal investigators at Scripps Research plan to synergize their deep-seated knowledge in vaccinology with AI-expertise at other institutes, chiefly Vanderbilt University. Collaborators at Vanderbilt University Medical Center will isolate alphavirus antibodies from people who have survived alphavirus-related infections, particularly those that protect against different alphaviruses. The team at Scripps Research will use these antibodies to guide vaccine design. Initially, they will determine the structure of antibodies and how they bind to alphaviruses.
“We need to understand where broadly protective antibodies attack and bind to the virus,” Schiffner says. “We can then use this information to design immunogens that focus antibodies onto regions conserved across alphaviruses.”
The team has already identified several such cross-protective antibodies, providing valuable blueprints for immunogen design.
“Normally, if you try to immunize with an entire virus, most of the antibodies will target regions that aren’t conserved among different viruses, so you get a vaccine that only works for a particular strain,” Schiffner explains. “There are very few regions that seem to be conserved across alphaviruses, and those are the regions that we want to target for broad protection against all alphaviruses.”
Next is testing various immunogen designs with computer models that include AI algorithms. If a design seems promising, it’s tested in vitro and in vivo.
But the role of AI doesn’t end there; data from ensuing in vitro and in vivo experimentation are fed back to the AI system, which can rapidly analyze antibody sequences, determine whether the immunogen is focusing antibodies on regions conserved across variants, and provide improved algorithms for reoptimizing the vaccine design.
“We’ll find out if the antibodies actually target the regions that they’re supposed to,” Schiffner says. “And once we get the AI results, we can use the information to improve our immunogen before the next stages; it’s an iterative process.”
The anticipated result: a broad vaccine that targets both encephalitic and arthritogenic alphaviruses that cause brain or joint inflammation, respectively. Moreover, the algorithms developed for this project could potentially be applied to other viruses, including influenza and HIV.
“But the main goal is to have an effective, broad vaccines for alphaviruses before they become a major problem.” emphasizes Schiffner.
For more information, contact press@scripps.edu

