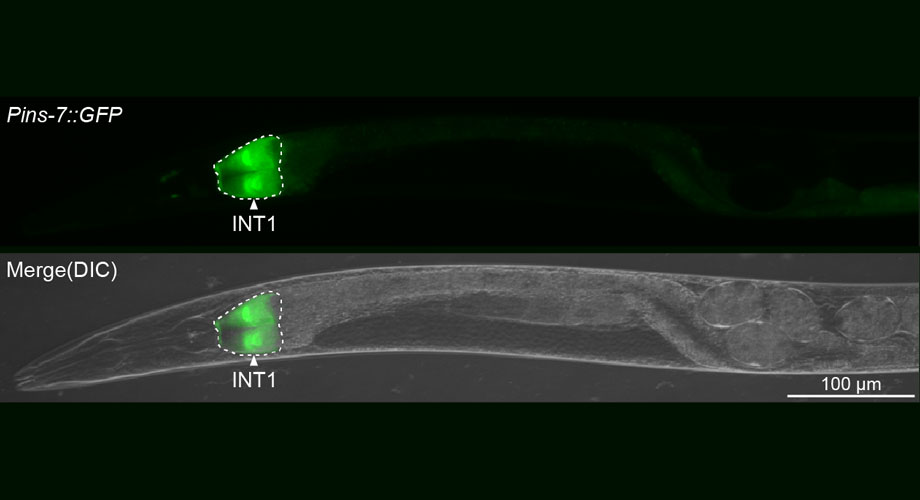
Scripps Research scientists discovered that specialized intestine cells (shown in green) in the C. elegans worm (gray) produce a peptide hormone that travels to the brain to control fat metabolism. Credit: Scripps Research
Gut molecule slows fat burning during fasting
Scripps Research scientists discovered a molecule produced by roundworm intestines that signals the brain to slow fat loss when food is not available.
August 21, 2024
LA JOLLA, CA—In a struggle that probably sounds familiar to dieters everywhere, the less a Caenorhabditis elegans (C. elegans) worm eats, the more slowly it loses fat. Now, scientists at Scripps Research have discovered why: a small molecule produced by the worms’ intestines during fasting travels to the brain to block a fat-burning signal during this time.
Although the exact molecule they identified in the worms has not yet been studied in humans, the new work helps scientists better understand the complex crosstalk between the gut and the brain. It also may shed light on why fasting—not eating for set periods of time—has benefits that are independent from the number of calories a person eats. The new study was published in Nature Communications on August 11, 2024.
“We’ve found for the first time that fasting is conveying information to the brain beyond just caloric withdrawal,” says Scripps Research Professor of Neuroscience Supriya Srinivasan, PhD, the senior author of the new study. “These findings make me wonder whether there are molecules made in the guts of other animals, including mammals, that explain some of the health outcomes associated with fasting.”
Researchers have long known that the brain controls the production and breakdown of fats in humans, other mammals and model organisms such as C. elegans. In 2017, Srinivasan’s group identified FLP-7, a brain hormone that triggers fat burning in the roundworm’s gut. However, C. elegans do not have sensory nerves in their intestines, so scientists have struggled to pin down the reverse communication pathway: How does the gut signal the brain?
“We knew that altering the metabolic state of the gut could change the properties of neurons in the brain, but it was very mysterious how this actually happened,” says Srinivasan.
In the new work, Srinivasan and her colleagues removed more than 100 signaling molecules from C. elegans intestines, one at a time, and measured their impact on the brain’s production of FLP-7. They found one molecule that had a large effect on FLP-7: a form of insulin known as INS-7. In humans, insulin is most known as the hormone produced by the pancreas that control blood sugar levels. But this insulin molecule was instead being made by gut cells and also impacting fat metabolism via the brain.
“When we first found that this was an insulin, we thought it was paradoxical,” recalls Srinivasan. “Insulin is so well studied in mammals, and there was no precedent for an insulin molecule having this role.”
However, when the group probed how INS-7 was impacting FLP-7-producing brain cells, they found that it was not activating insulin receptors—as all previously discovered insulin molecules do—but by blocking the insulin receptor. In turn, this blockade set off a cascade of other molecular events that eventually made the brain cells stop producing FLP-7.
“INS-7 is basically a signal coming from the intestines that tells the brain not to burn any more fat stores right now because there’s no food coming in,” explains Srinivasan.
Studies have previously shown that periods of fasting can influence the body in a variety of ways, but the mechanisms of those changes have been unclear. The new study points toward one way that an empty gut can signal the brain, which could potentially lead to a variety of health impacts beyond fat.
The new results, Srinivasan says, help explain how the brain and digestive system communicate in both directions to control metabolism based on the availability of food. More research is needed to uncover which specific pathways are involved in new gut-to-brain signals in mammals. Compounds that mimic gut hormones—such as semaglutide, commonly known under brand names such as Ozempic, Wegovy and Rybelus—have recently emerged as popular ways to control obesity and diabetes, so new gut peptides could add to this drug class. Srinivasan is also planning experiments to probe how C. elegans gut cells are triggered to produce INS-7 during fasting and which types of brain cells are affected by the molecule.
In addition to Srinivasan, authors of the study, “A homeostatic gut-to-brain insulin antagonist restrains neuronally stimulated fat loss,” are Chung-Chih Liu, Ayub Khan, Nicolas Seban, Nicole Littlejohn, and Aayushi Shah of Scripps Research.
This work was supported by funding from the National Institutes of Health (R01 DK124706 and R01 AG056648).
For more information, contact press@scripps.edu