
Graduate student Jessica Bush, research associate Haruo Aikawa, PhD, and Chemistry Professor Matthew Disney, PhD, go over assays used to find RNA-binding molecules to fight C9 ALS/FTD at their lab at Scripps Research in Jupiter, Florida.
Potential treatment for ALS, frontotemporal dementia targets RNA
Compound co-opts a natural enzyme to degrade a deadly disease at its source, erasing 70 percent of a toxic protein in mice.
October 27, 2021
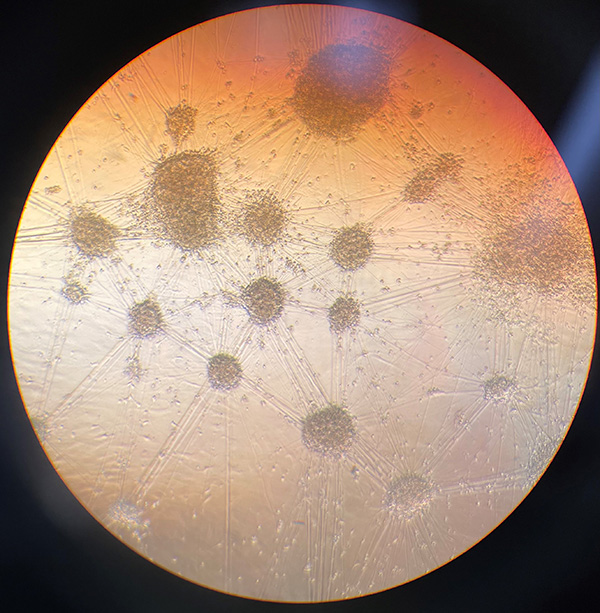
To study the effectiveness of RNA-targeting compounds aimed at treating C9 ALS/FTD, the scientists directed cells from patients with the disease to become stem cells and then specialize into nerve cells. Photo credit: Jessica Bush, Disney Lab at Scripps Research
JUPITER, FL—One of the most commonly inherited forms of ALS and frontotemporal dementia is referred to as C9 ALS/FTD, so named for the repeated section of DNA on chromosome 9 that causes it.
A collaboration led by scientists at Scripps Research in Florida has successfully treated the genetic disease in mice, with a potential drug molecule engineered in the lab of chemist Matthew Disney, PhD. The compound works in a new way, by directing the cell’s own immune machinery to degrade and eliminate the disease-causing RNA. The team’s study is published Wednesday in the journal Science Translational Medicine. Collaborators include Leonard Petrucelli, PhD, of the Mayo Clinic in Jacksonville, and Jeffrey Rothstein, MD, PhD, of Johns Hopkins University in Baltimore.
One disease, many symptoms
Also known as Lou Gehrig’s disease, ALS causes progressive loss of motor neurons, the elongated nerve cells that connect muscles to the central nervous system. As motor neurons die, paralysis, muscle loss, swallowing and eventually, breathing difficulties develop, leading ultimately to death. Scientists are learning that ALS has multiple causes, some of them sporadic, and some inherited or familial.
Frontotemporal dementia similarly has both familial and sporadic causes. It involves progressive damage to neurons in the brain’s frontal and temporal lobes. Symptoms may include difficulty walking or odd behavioral and emotional states. Like ALS, there is no cure for frontotemporal dementia.
While people with FTD appear outwardly to have a completely different illness than people with ALS, those whose condition is caused by the C9 genetic repeat have the same disease. Manifestations differ according to cell types affected. The more times the sequence repeats, the earlier and more severe the disease symptoms.
The disease-causing mutations involve repeats of the nucleotides guanine and cytosine, specifically repeats of GGGGCC segments on chromosome 9, open reading frame 72. The number of disease-causing repeats can range from around 60 into the thousands. People who inherit the diseased gene can develop ALS, FTD or both. Studies have estimated that around 1 in 5 people diagnosed with familial ALS, and around 1 in 10 people with familial FTD carry the C9 mutations. The average age of symptom onset is 58.
“This is a disease that runs in families. Based on the number of repeats, doctors can assess whether a patient would be affected with the disease. So, you know before a patient has symptoms that they have a high likelihood of developing it, and yet there is no treatment,” Disney says. “That makes it even more imperative to develop strategies to that could create a medicine.”
A team effort
To assess the effectiveness of their compounds, the team needed both diagnostic biomarkers and patient-derived neurons displaying the C9 mutations. The Petrucelli group at Mayo Clinic has extensively studied C9 ALS/FTD and developed the diagnostic biomarkers. The Rothstein group at Johns Hopkins treats and researches ALS and provided stem cells, which the Disney Lab then brought forward into neurons that displayed the diseased array of GGGGCC repeats.
In their research, Disney’s team designed a compound that targeted the RNA that causes the disease. The compound causes an interaction between the RNA and pathways that a cell uses to eliminate RNAs. The compound eliminated 70 percent of the toxic protein fragments from mice bread to have the disease, and removed most hallmarks of the disease from the patient-derived nerve cells.
A single injection in the mice showed benefit through the entire length of the study period, which was six weeks, says Jessica Bush, a Scripps Research graduate student who was the paper’s first author.
“I think that it’s so exciting that we can look at a disease like ALS, and by taking a different approach or new perspective, we can open the door to a whole new world of possibilities, and start down the road toward therapies,” Bush says.
Basic science behind the discovery
Disney designed the compound by applying nearly 15 years of his group’s research on finding druggable structures on RNA, a notoriously changeable and transient molecule, and building a library of compounds able to bind those druggable structures.
The successful compound works by binding tightly to the disease-causing RNA in multiple places, while also attracting an enzyme that eliminates RNAs. Nature apparently created the degrading enzyme to defend cells from viral infection and provide quality control for protein production.
“We co-opt a natural process to eliminate disease-causing RNA,” Disney says. “A full analysis of the RNAs in the cells treated with the compound showed it was very specific and selective.”
Moving the technology forward to where it can be tested in humans requires a large amount of additional tests and refinements, a process that may take several years, Disney adds.
“These studies, we hope, will advance new ways of targeting the RNA that causes ALS as well as other diseases,” he says. “There is a possibility here to eventually treat these patients before they develop symptoms, but it will be a long road before reaching the clinic.”
In addition to Disney, Bush, Petrucelli and Rothstein, the authors of the study, “Ribonuclease recruitment using a small molecule reduced c9ALS/FTD r(G4C2) repeat expansion in vitro and in vivo ALS models,” include the following contributors: From Scripps Research, Haruo Aikawa, Rita Fuerst, Yue Li, Andrei Ursu, Samantha M. Meyer, Raphael I. Benhamou, Jonathan Chen, Tanya Khan, Sarah Wagner-Griffin, Montina Van Meter, Yuquan Tong and Jessica Childs-Disney. From the University of Florida in Gainesville, Hailey Olafson, Kendra McKee and Eric Wang. From the Mayo Clinic in Jacksonville, Tania Gendron and Yongjie Zhang. From Johns Hopkins University in Baltimore, Alyssa N. Coyne. From Florida Atlantic University, Ilyas Yildirim and Kye Won Wang.
Funding for the study was provided by the National Institutes of Health NIH, P01 NS099114 DP1, NS096898, R35 NS116846, R35 NS097273, Target ALS, the Nelson Family Fund, the Family First Fund, the Deutsche Forschungsgemeinschaft DFG Postdoctoral Fellowship, and the ALS Association Milton Safenowitz Postdoctoral Fellowship.
For more information, contact press@scripps.edu

