
Painting by Scripps Research professor David S. Goodsell, PhD*
Scripps Research scientists tackle COVID-19 coronavirus pandemic from many angles
Ongoing studies reveal important information about how the virus spreads and infects the body, and point to different approaches for potential vaccines and medicines.
March 18, 2020
Scripps Research scientists are pursuing multiple lines of research aimed at understanding and helping to mitigate the impact of the novel coronavirus behind the COVID-19 epidemic that has spread across the globe. They are tracing how the virus originated and spreads, exploring how it invades the body and how the immune system responds, and working to develop potential vaccines and medicines against the virus.
What is coronavirus?
Coronavirus is the family of viruses that causes outbreaks of severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), two illnesses that emerged within the last two decades. Symptoms of coronavirus infections include flu-like symptoms such as fever, cough and shortness of breath.
The virus behind the current epidemic, called SARS-CoV-2, is a previously unknown member of the coronavirus family. The epidemic, which began in the Chinese city of Wuhan, has spread to every continent but Antarctica and has sickened tens of thousands of people, resulting in several thousand deaths as of early March 2020.
How did this virus originate, and how does it spread?
Kristian Andersen, PhD, a Scripps Research genomic epidemiologist and professor in the Department of Immunology and Microbiology, is tracing the origins of the novel coronavirus genome based on public sequencing data. An expert in tracking the spread of deadly viruses (including Ebola, Lassa and Zika), Andersen launched a collaboration with institutes from around the world to analyze the virus’s genome and trace its origins. The team’s study, reported in Nature Medicine on March 17, quells rumors about that it was engineered in a laboratory. You can read more about the findings here.
His team is also working with colleagues across the globe to better understand how the virus is transmitting in the human population—from its beginning in China to its current spread around the world.
Can we repurpose existing drugs to treat patients with COVID-19?
Scripps Research teams are testing already approved drugs and compounds with significant safety data in humans available, for activity against SARS-CoV-2. These drugs could be made available to treat coronavirus patients on a much quicker timescale than novel therapies.
Calibr, the drug development division of Scripps Research, is leveraging a unique resource, the ReFRAME drug repurposing collection. With support from the Bill & Melinda Gates Foundation, Calibr compiled ReFRAME, the world’s leading collection of known drugs comprising over 14,000 compounds that have been approved by the FDA for other diseases or have been tested for human safety. Calibr also developed an open source database containing preclinical and clinical data on these compounds. Since information on the drugs’ therapeutic properties and safety is known, they can be screened and rapidly advanced into the clinic.
Since its creation in 2018, ReFRAME has been distributed broadly to nonprofit collaborators for global health and used to identify repurposing opportunities for a range of diseases. When the COVID-19 outbreak began, Calibr was able to mobilize ReFRAME quickly to begin searching for existing drugs and other compounds that might be repurposed against the coronavirus.
ReFRAME is now being screened to identify compounds that can:
- Prevent the virus from entering and infecting cells
- Prevent the virus from replicating in cells
- Augment the efficacy of antivirals such as remdesivir, which is being tested in five COVID-19 clinical trials
Since the outbreak began, Calibr has established collaborations to screen the ReFRAME library for potential coronavirus therapies with nine outside research teams, including U.S. laboratories in Maryland, Massachusetts, New York, and Texas, as well as overseas labs in the UK, Germany, Belgium and Hong Kong. Calibr is also establishing partnerships with pharmaceutical companies to screen earlier stage antiviral collections against COVID-19.
ReFRAME has been highlighted in the COVID-19 Therapeutics Accelerator launched by the Bill & Melinda Gates Foundation.
In addition to Calibr, Matthew Disney, PhD, a chemistry professor the Florida campus of Scripps Research, is also exploring compound repurposing. Disney develops potential medicines that work by precisely targeting disease-causing RNA, the protein-building machinery inside of cells. He is using his tools to identify drug-like compounds that may have activity against the novel coronavirus, which is an RNA virus.
How does the novel coronavirus interact with our immune system? Can this knowledge help us fight the virus and develop a vaccine?
Researchers in the Scripps Research laboratory of Dennis Burton, PhD, chair of the Department of Immunology and Microbiology, are studying the human immune response to SARS-CoV-2 infections. They are also working to identify potent “broadly neutralizing antibodies,” which might serve as the basis for vaccines or antiviral therapies against COVID-19.
The laboratory of Ian Wilson, DPhil, chair of the Department of Integrative Structural and Computational Biology at Scripps Research, is studying the differences between the virus that caused the 2002 outbreak of SARS (SARS-CoV) and the novel coronavirus (SARS-CoV-2) behind the COVID-19 pandemic. They are exploring whether antibodies produced against one coronavirus can interact with a different coronavirus.
They found that one antibody (CR3022), previously produced against SARS-CoV by the company Crucell Holland BV, binds to the receptor binding domain on the spike protein of SARS-CoV-2. Wilson’s team produced the first 3D structure of the SARS-CoV-2 receptor binding domain bound with the CR3022 antibody that neutralizes SARS-CoV. In another collaboration with the University of Hong Kong, cross reactive antibody responses were found between SARS-CoV-2 and SARS-CoV infection.
The Wilson lab plans to work on structures of antibodies isolated from recovering COVID-19 patients when they become available from researchers at medical research centers. The findings of these studies are producing critical information for researchers worldwide as they seek to develop vaccines to SARS-CoV-2.
Andrew Ward, PhD, a professor of Integrative Structural and Computational Biology at Scripps Research, has a longstanding interest in understanding immune responses to coronaviruses, particularly how the body responds to the surface spike protein on the virus. Ward’s team revealed the first structure of a human coronavirus spike protein in 2017 from the HKU1 virus, and subsequently went on to describe spike proteins from SARS and MERS—the latter when it was connected with a neutralizing antibody. They are now investigating the structure of the SARS-CoV-2 spike protein and working with collaborators in the United States who are isolating antibodies from infected patients. Lastly, Ward’s group has developed new imaging methods that work as a diagnostic tool to directly probe blood samples from infected patients.
What are approaches being taken to develop novel vaccines against coronavirus?
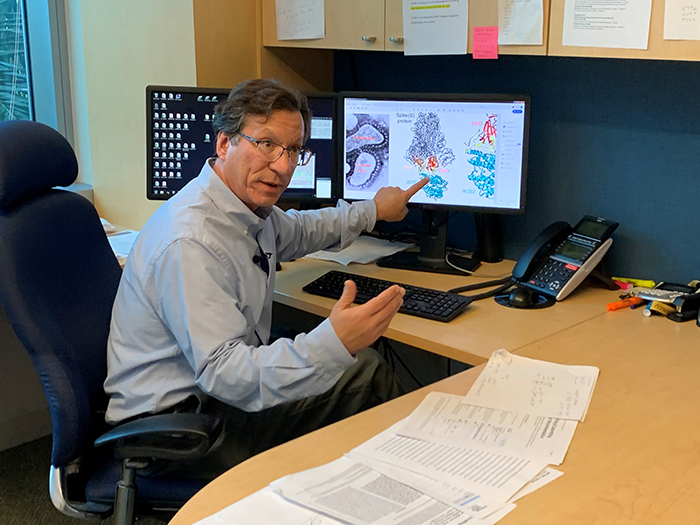
Scripps Research professor Michael Farzan, PhD in his office on the Jupiter, FL campus of Scripps Research.
Scripps Research professors Michael Farzan, PhD, and Hyeryun Choe, PhD, both in the Department of Immunology and Microbiology, study how the SARS-CoV-2 virus infects cells. Their goal is to develop optimal vaccine approaches, and to advance rapid development of antiviral drugs and biologic therapies.
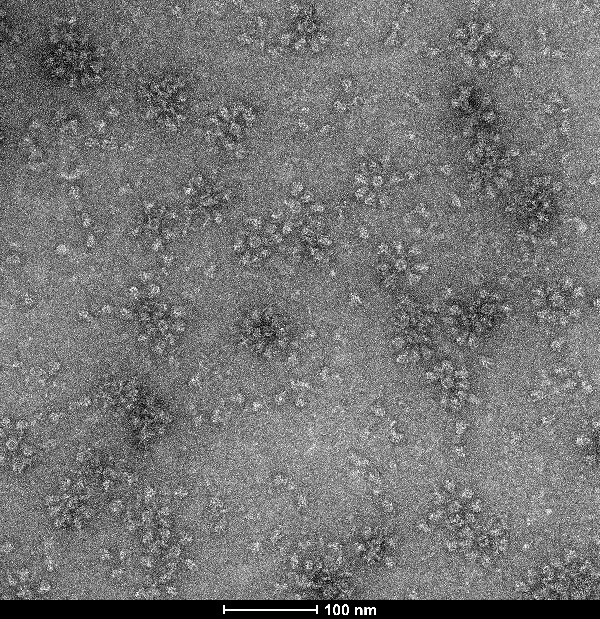
Electron microscopy image of unpurified SARS-CoV-2 nanoparticles. Courtesy: Jiang Zhu, PhD
Jiang Zhu, PhD, an associate professor in the Department of Integrative Structural and Computational Biology at Scripps Research, has developed a patented technology for engineering vaccines built with tiny fragments of protein nanoparticles. Zhu and coworkers have developed a self-assembling prototype that features SARS-CoV-2 protein spikes protruding from the protein nanoparticle scaffold that could stimulate a strong immune system response in cells to protect against a real SARS-CoV-2 virus.
*About the cover image: This painting, by Scripps Research professor David S. Goodsell, PhD, depicts a coronavirus just entering the lungs, surrounded by mucus secreted by respiratory cells, secreted antibodies, and several small immune systems proteins. The virus is enclosed by a membrane that includes the S (spike) protein, which will mediate attachment and entry into cells, M (membrane) protein, which is involved in organization of the nucleoprotein inside, and E (envelope) protein, which is a membrane channel involved in budding of the virus and may be incorporated into the virion during that process. The nucleoprotein inside includes many copies of the N (nucleocapsid) protein bound to the genomic RNA.
Media interested in interviewing these Scripps Research scientists can contact Chris Emery, Sr. Director of Communications, at cemery@scripps.edu.
For more information, contact press@scripps.edu

